Your two kidneys are vital organs that perform many functions to keep your blood clean and chemically balanced. Understanding how your kidneys work can help you to keep them healthy.
What do my kidneys do?
The kidneys remove wastes and extra water from the blood to form urine. Urine flows from the kidneys to the bladder through the ureters.
Your kidneys are bean-shaped organs, each about the size of your fist. They are located near the middle of your back, just below the rib cage. The kidneys are sophisticated reprocessing machines. Every day, your kidneys process about 200 quarts of blood to sift out about 2 quarts of waste products and extra water. The waste and extra water become urine, which flows to your bladder through tubes called ureters. Your bladder stores urine until you go to the bathroom.
The wastes in your blood come from the normal breakdown of active tissues and from the food you eat. Your body uses the food for energy and self-repair. After your body has taken what it needs from the food, waste is sent to the blood. If your kidneys did not remove these wastes, the wastes would build up in the blood and damage your body.
The actual filtering occurs in tiny units inside your kidneys called nephrons. Every kidney has about a million nephrons. In the nephron, a glomerulus—which is a tiny blood vessel, or capillary—intertwines with a tiny urine-collecting tube called a tubule. A complicated chemical exchange takes place, as waste materials and water leave your blood and enter your urinary system.
At first, the tubules receive a combination of waste materials and chemicals that your body can still use. Your kidneys measure out chemicals like sodium, phosphorus, and potassium and release them back to the blood to return to the body. In this way, your kidneys regulate the body’s level of these substances. The right balance is necessary for life, but excess levels can be harmful.

In the nephron (left), tiny blood vessels intertwine with urine-collecting tubes. Each kidney contains about 1 million nephrons.
In addition to removing wastes, your kidneys release three important hormones:
- erythropoietin (eh-RITH-ro-POY-eh-tin), or EPO, which stimulates the bone marrow to make red blood cells
- renin (REE-nin), which regulates blood pressure
- calcitriol (kal-suh-TRY-ul), the active form of vitamin D, which helps maintain calcium for bones and for normal chemical balance in the body
What is renal function?
Your health care team may talk about the work your kidneys do as renal function. If you have two healthy kidneys, you have 100 percent of your renal function. This is more renal function than you really need. Some people are born with only one kidney, and these people are able to lead normal, healthy lives. Many people donate a kidney for transplantation to a family member or friend. Small declines in renal function may not cause a problem.
But many people with reduced renal function have a kidney disease that will get worse. You will have serious health problems if you have less than 25 percent of your renal function. If your renal function drops below 10 to 15 percent, you cannot live long without some form of renal replacement therapy—either dialysis or transplantation.
Why do kidneys fail?
Most kidney diseases attack the nephrons, causing them to lose their filtering capacity. Damage to the nephrons may happen quickly, often as the result of injury or poisoning. But most kidney diseases destroy the nephrons slowly and silently. Only after years or even decades will the damage become apparent. Most kidney diseases attack both kidneys simultaneously.
The two most common causes of kidney disease are diabetes and high blood pressure. If your family has a history of any kind of kidney problems, you may be at risk for kidney disease.
Diabetic Nephropathy
Diabetes is a disease that keeps the body from using glucose (sugar) as it should. If glucose stays in your blood instead of breaking down, it can act like a poison. Damage to the nephrons from unused glucose in the blood is called diabetic nephropathy. If you keep your blood glucose levels down, you can delay or prevent diabetic nephropathy.
High Blood Pressure
High blood pressure can damage the small blood vessels in your kidneys. The damaged vessels cannot filter wastes from your blood as they are supposed to.
Your doctor may prescribe blood pressure medication. Blood pressure medicines called angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) have been found to protect the kidneys even more than other medicines that lower blood pressure to similar levels. The National Heart, Lung, and Blood Institute (NHLBI), one of the National Institutes of Health, recommends that people with diabetes or reduced kidney function should keep their blood pressure below 130/80 mm Hg.
Glomerular Diseases
Several different types of kidney disease are grouped together under this category, including autoimmune diseases, infection-related diseases, and sclerotic diseases. As the name indicates, glomerular diseases attack the tiny blood vessels (glomeruli) within the kidney. The most common primary glomerular diseases include membranous nephropathy, IgA nephropathy, and focal segmental glomerulosclerosis. Protein, blood, or both in the urine are often the first signs of these diseases. They can slowly destroy kidney function. Blood pressure control is important with any kidney disease. Treatments for glomerular diseases may include immunosuppressive drugs or steroids to reduce inflammation and proteinuria, depending on the specific disease.
Inherited and Congenital Kidney Diseases
Some kidney diseases result from hereditary factors. Polycystic kidney disease (PKD), for example, is a genetic disorder in which many cysts grow in the kidneys. PKD cysts can slowly replace much of the mass of the kidneys, reducing kidney function and leading to kidney failure.
Some kidney problems may show up when a child is still developing in the womb. Examples include autosomal recessive PKD, a rare form of PKD, and other developmental problems that interfere with the normal formation of the nephrons. The signs of kidney disease in children vary. A child may grow unusually slowly, may vomit often, or may have back or side pain. Some kidney diseases may be “silent” for months or even years.
If your child has a kidney disease, your child’s doctor should find it during a regular checkup. Be sure your child sees a doctor regularly. The first sign of a kidney problem may be high blood pressure, a low number of red blood cells (anemia), or blood or protein in the child’s urine. If the doctor finds any of these problems, further tests may be necessary, including additional blood and urine tests or radiology studies. In some cases, the doctor may need to perform a biopsy—removing a tiny piece of the kidney to examine under a microscope.
Some hereditary kidney diseases may not be detected until adulthood. The most common form of PKD was once called "adult PKD" because the symptoms of high blood pressure and renal failure usually do not occur until patients are in their twenties or thirties. But with advances in diagnostic imaging technology, doctors have found cysts in children and adolescents before any symptoms appear.
Other Causes of Kidney Disease
Poisons and trauma, for example a direct and forceful blow to your kidneys, can lead to kidney disease.
Some over-the-counter medicines can be poisonous to your kidneys if taken regularly over a long period of time. Products that combine aspirin, acetaminophen, and other medicines such as ibuprofen have been found to be the most dangerous to the kidneys. If you take painkillers regularly, check with your doctor to make sure you are not putting your kidneys at risk.
How do kidneys fail?
Many factors that influence the speed of kidney failure are not completely understood. Researchers are still studying how protein in the diet and cholesterol levels in the blood affect kidney function.
Acute Renal Failure
Some kidney problems happen quickly, like an accident that injures the kidneys. Losing a lot of blood can cause sudden kidney failure. Some drugs or poisons can make your kidneys stop working. These sudden drops in kidney function are called acute renal failure (ARF).
ARF may lead to permanent loss of kidney function. But if your kidneys are not seriously damaged, acute renal failure may be reversed.
Chronic Kidney Disease
Most kidney problems, however, happen slowly. You may have “silent” kidney disease for years. Gradual loss of kidney function is called chronic kidney disease (CKD) or chronic renal insufficiency. People with CKD may go on to permanent kidney failure. They also have a high risk of dying from a stroke or heart attack.
End-Stage Renal Disease
Total or nearly total and permanent kidney failure is called end-stage renal disease (ESRD). People with ESRD must undergo dialysis or transplantation to stay alive.
What are the signs of kidney disease?
People in the early stages of kidney disease usually do not feel sick at all.
If your kidney disease gets worse, you may need to urinate more often or less often. You may feel tired or itchy. You may lose your appetite or experience nausea and vomiting. Your hands or feet may swell or feel numb. You may get drowsy or have trouble concentrating. Your skin may darken. You may have muscle cramps.
What medical tests will my doctor use to detect kidney disease?
Since you can have kidney disease without any symptoms, your doctor may first detect the condition through routine blood and urine tests. The National Kidney Foundation recommends three simple tests to screen for kidney disease: a blood pressure measurement, a spot check for protein or albumin in the urine (proteinuria), and a calculation of glomerular filtration rate (GFR) based on a serum creatinine measurement. Measuring urea nitrogen in the blood provides additional information.
Blood Pressure Measurement
disease. It can also be a sign that your kidneys are already impaired. The only way to know whether your blood pressure is high is to have a health professional measure it with a blood pressure cuff. The result is expressed as two numbers. The top number, which is called the systolic pressure, represents the pressure when your heart is beating. The bottom number, which is called the diastolic pressure, shows the pressure when your heart is resting between beats. Your blood pressure is considered normal if it stays below 120/80 (expressed as “120 over 80”). The NHLBI recommends that people with kidney disease use whatever therapy is necessary, including lifestyle changes and medicines, to keep their blood pressure below 130/80.
Microalbuminuria and Proteinuria
Healthy kidneys take wastes out of the blood but leave protein. Impaired kidneys may fail to separate a blood protein called albumin from the wastes. At first, only small amounts of albumin may leak into the urine, a condition known as microalbuminuria, a sign of deteriorating kidney function. As kidney function worsens, the amount of albumin and other proteins in the urine increases, and the condition is called proteinuria. Your doctor may test for protein using a dipstick in a small sample of your urine taken in the doctor’s office. The color of the dipstick indicates the presence or absence of proteinuria.
A more sensitive test for protein or albumin in the urine involves laboratory measurement and calculation of the protein-to-creatinine or albumin-to-creatinine ratio. This test should be used to detect kidney disease in people at high risk, especially those with diabetes. If your first laboratory test shows high levels of protein, another test should be done 1 to 2 weeks later. If the second test also shows high levels of protein, you have persistent proteinuria and should have additional tests to evaluate your kidney function.
Glomerular Filtration Rate (GFR) Based on Creatinine Measurement
GFR is a calculation of how efficiently the kidneys are filtering wastes from the blood. A traditional GFR calculation requires an injection into the bloodstream of a substance that is later measured in a 24-hour urine collection. Recently, scientists found they could calculate GFR without an injection or urine collection. The new calculation requires only a measurement of the creatinine in a blood sample.
Creatinine is a waste product in the blood created by the normal breakdown of muscle cells during activity. Healthy kidneys take creatinine out of the blood and put it into the urine to leave the body. When kidneys are not working well, creatinine builds up in the blood.
In the lab, your blood will be tested to see how many milligrams of creatinine are in one deciliter of blood (mg/dL). Creatinine levels in the blood can vary, and each laboratory has its own normal range, usually 0.6 to 1.2 mg/dL. If your creatinine level is only slightly above this range, you probably will not feel sick, but the elevation is a sign that your kidneys are not working at full strength. One formula for estimating kidney function equates a creatinine level of 1.7 mg/dL for most men and 1.4 mg/dL for most women to 50 percent of normal kidney function. But because creatinine values are so variable and can be affected by diet, a GFR calculation is more accurate for determining whether a person has reduced kidney function.
The new GFR calculation uses the patient’s creatinine measurement along with weight, age, and values assigned for sex and race. Some medical laboratories may make the GFR calculation when a creatinine value is measured and include it on their lab report.
Blood Urea Nitrogen (BUN)
Blood carries protein to cells throughout the body. After the cells use the protein, the remaining waste product is returned to the blood as urea, a compound that contains nitrogen. Healthy kidneys take urea out of the blood and put it in the urine. If your kidneys are not working well, the urea will stay in the blood.
A deciliter of normal blood contains 7 to 20 milligrams of urea. If your BUN is more than 20 mg/dL, your kidneys may not be working at full strength. Other possible causes of an elevated BUN include dehydration and heart failure.
Additional Tests for Kidney Disease
If blood and urine tests indicate reduced kidney function, your doctor may recommend additional tests to help identify the cause of the problem.
Renal imaging. Methods of renal imaging (taking pictures of the kidneys) include ultrasound, computed tomography (CT scan), and magnetic resonance imaging (MRI). These tools are most helpful in finding unusual growths or blockages to the flow of urine.
Renal biopsy. Your doctor may want to see a tiny piece of your kidney tissue under a microscope. To obtain this tissue sample, the doctor will perform a renal biopsy—a hospital procedure in which the doctor inserts a needle through your skin into the back of the kidney. The needle retrieves a strand of tissue about 1/2 to 3/4 of an inch long. For the procedure, you will lie on your stomach on a table and receive local anesthetic to numb the skin. The sample tissue will help the doctor identify problems at the cellular level.
For more information, see the fact sheet on Kidney Biopsy from the National Kidney and Urologic Diseases Information Clearinghouse.
What are the stages of kidney disease?
Your GFR is the best indicator of how well your kidneys are working. In 2002, the National Kidney Foundation published treatment guidelines that identified five stages of CKD based on declining GFR measurements. The guidelines recommend different actions based on the stage of kidney disease.
- Increased risk of CKD. A GFR of 90 or above is considered normal. Even with a normal GFR, you may be at increased risk for developing CKD if you have diabetes, high blood pressure, or a family history of kidney disease. The risk increases with age: People over 65 are more than twice as likely to develop CKD as people between the ages of 45 and 65. African Americans also have a higher risk of developing CKD.
- Stage 1: Kidney damage with normal GFR (90 or above). Kidney damage may be detected before the GFR begins to decline. In this first stage of kidney disease, the goals of treatment are to slow the progression of CKD and reduce the risk of heart and blood vessel disease.
- Stage 2: Kidney damage with mild decrease in GFR (60 to 89). When kidney function starts to decline, your health care provider will estimate the progression of your CKD and continue treatment to reduce the risk of other health problems.
- Stage 3: Moderate decrease in GFR (30 to 59). When CKD has advanced to this stage, anemia and bone problems become more common. Work with your health care provider to prevent or treat these complications.
- Stage 4: Severe reduction in GFR (15 to 29). Continue following the treatment for complications of CKD and learn as much as you can about the treatments for kidney failure. Each treatment requires preparation. If you choose hemodialysis, you will need to have a procedure to make a vein in your arm larger and stronger for repeated needle insertions. For peritoneal dialysis, you will need to have a catheter placed in your abdomen. Or you may want to ask family or friends to consider donating a kidney for transplantation.
- Stage 5: Kidney failure (GFR less than 15). When the kidneys do not work well enough to maintain life, you will need dialysis or a kidney transplant.
In addition to tracking your GFR, blood tests can show when substances in your blood are out of balance. If phosphorus or potassium levels start to climb, a blood test will prompt your health care provider to address these issues before they permanently affect your health.
What can I do about kidney disease?
Unfortunately, chronic kidney disease often cannot be cured. But if you are in the early stages of a kidney disease, you may be able to make your kidneys last longer by taking certain steps. You will also want to be sure that risks for heart attack and stroke are minimized, since CKD patients are susceptible to these problems.
- If you have diabetes, watch your blood glucose closely to keep it under control. Consult your doctor for the latest in treatment.
- Avoid pain pills that may make your kidney disease worse. Check with your doctor before taking any medicine.
Blood Pressure
People with reduced kidney function (a high creatinine level in the blood or a low creatinine clearance) should have their blood pressure controlled, and an ACE inhibitor or an ARB should be one of their medications. Many people will require two or more types of medication to keep their blood pressure below 130/80 mm Hg. A diuretic is an important addition to the ACE inhibitor or ARB.
Diet
People with reduced kidney function need to be aware that some parts of a normal diet may speed their kidney failure.
Protein. Protein is important to your body. It helps your body repair muscles and fight disease. Protein comes mostly from meat. As discussed in an earlier section, healthy kidneys take wastes out of the blood but leave protein. Impaired kidneys may fail to separate the protein from the wastes.
Some doctors tell their kidney patients to limit the amount of protein they eat so that the kidneys have less work to do. But you cannot avoid protein entirely. You may need to work with a dietitian to find the right food plan.
Cholesterol. Another problem that may be associated with kidney failure is too much cholesterol (koh-LES-tuh-rawl) in your blood. High levels of cholesterol may result from a high-fat diet.
Cholesterol can build up on the inside walls of your blood vessels. The buildup makes pumping blood through the vessels harder for your heart and can cause heart attacks and strokes.
Smoking. Smoking not only increases the risk of kidney disease, it contributes to deaths from strokes and heart attacks in people with CKD. You should try your best to stop smoking.
Sodium. Sodium is a chemical found in salt and other foods. Sodium in your diet may raise your blood pressure, so you should limit foods that contain high levels of sodium. High-sodium foods include canned or processed foods like frozen dinners and hot dogs.
Potassium. Potassium is a mineral found naturally in many fruits and vegetables, like oranges, potatoes, bananas, dried fruits, dried beans and peas, and nuts. Healthy kidneys measure potassium in your blood and remove excess amounts. Diseased kidneys may fail to remove excess potassium, and with very poor kidney function, high potassium levels can affect the heart rhythm.
Treating Anemia
Anemia is a condition in which the blood does not contain enough red blood cells. These cells are important because they carry oxygen throughout the body. If you are anemic, you will feel tired and look pale. Healthy kidneys make the hormone EPO, which stimulates the bones to make red blood cells. Diseased kidneys may not make enough EPO. You may need to take injections of a man-made form of EPO.
Preparing for End-Stage Renal Disease
As your kidney disease progresses, you will need to make several decisions. You will need to learn about your options for treating ESRD so that you can make an informed choice between hemodialysis, peritoneal dialysis, and transplantation.
What happens if my kidneys fail completely?
Complete and irreversible kidney failure is sometimes called end-stage renal disease, or ESRD. If your kidneys stop working completely, your body fills with extra water and waste products. This condition is called uremia. Your hands or feet may swell. You will feel tired and weak because your body needs clean blood to function properly.
Untreated uremia may lead to seizures or coma and will ultimately result in death. If your kidneys stop working completely, you will need to undergo dialysis or kidney transplantation.
Dialysis
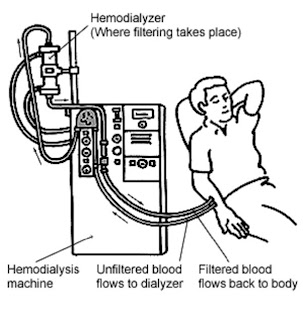
The two major forms of dialysis are hemodialysis and peritoneal dialysis. In hemodialysis, your blood is sent through a filter that removes waste products. The clean blood is returned to your body. Hemodialysis is usually performed at a dialysis center three times per week for 3 to 4 hours.
Hemodialysis
In peritoneal dialysis, a fluid is put into your abdomen. This fluid captures the waste products from your blood. After a few hours, the fluid containing your body’s wastes is drained away. Then, a fresh bag of fluid is dripped into the abdomen. Patients can perform peritoneal dialysis themselves. Patients using continuous ambulatory peritoneal dialysis (CAPD) change fluid four times a day. Another form of peritoneal dialysis, called continuous cycling peritoneal dialysis (CCPD), can be performed at night with a machine that drains and refills the abdomen automatically
Peritoneal dialysis
 Kidney Transplantation
Kidney Transplantation
A donated kidney may come from an anonymous donor who has recently died or from a living person, usually a relative. The kidney that you receive must be a good match for your body. The more the new kidney is like you, the less likely your immune system is to reject it. Your immune system protects you from disease by attacking anything that is not recognized as a normal part of your body. So your immune system will attack a kidney that appears too “foreign.” You will take special drugs to help trick your immune system so it does not reject the transplanted kidney.
Hope through Research
As our understanding of the causes of kidney failure increases, so will our ability to predict and prevent these diseases. Recent studies have shown that intensive control of diabetes and high blood pressure can prevent or delay the onset of kidney disease.
In the area of genetics, researchers supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) have located two genes that cause the most common form of PKD and learned that a person must have two defective copies of the PKD1 gene to develop PKD. Researchers have also found a gene in the roundworm that is identical to the PKD1 gene. This new knowledge will be used in the search for effective therapies to prevent or treat PKD.
In the area of transplantation, new drugs to help the body accept foreign tissue increase the likelihood that a transplanted kidney will survive and function properly. Scientists at NIDDK are also developing new techniques to induce tolerance for foreign tissue in patients before they receive transplanted organs. This technique will eliminate or reduce the need for immunosuppressive drugs and thereby reduce expense and complications. In the future, scientists may develop an artificial kidney for implantation.
Points to Remember
- Your kidneys are vital organs that keep your blood clean and chemically balanced.
- The progression of kidney disease can be slowed, but it cannot always be reversed.
- End-stage renal disease (ESRD) is the total loss of kidney function.
- Dialysis and transplantation can extend the lives of people with ESRD.
- Diabetes and high blood pressure are the two leading causes of kidney failure.
- You should see a nephrologist regularly if you have renal disease.
- Chronic kidney disease (CKD) increases the risk of heart attacks and strokes.
- If you are in the early stages of renal disease, you may be able to save your remaining renal function for many years by
- controlling your blood glucose
- controlling your blood pressure
- following a low-protein diet
- maintaining healthy levels of cholesterol in your blood
- taking an ACE inhibitor or an ARB
- quitting smoking